

Discover more from Real Gaijin
Brush with Disaster during the Tail End of Japan’s Golden Week
First-hand account of my week-long stay of being poked, prodded, and pricked at a Japanese hospital to recover from a life-threatening illness.
What’s new: Recently I directly experienced a potentially serious condition called cellulitis, a bacterial skin infection called hoka shikien (蜂窩織炎) in Japanese. In my case it caused severe pain, swelling, and inflammation of the lower part of my right leg. These symptoms developed suddenly under mysterious circumstances and caused large patches of skin in the area to turn bright red and feel hot to the touch—actually it was like my leg was on fire. While this has never happened to me, I suppose that the pain would be similar to getting one’s leg caught in a trap for wild animals. As cellulitis is commonly caused by staphylococcus and streptococcus bacteria that are normally present on the surface of everyone’s skin, some microscopic piece of such bacteria must have found its way into my body through a break in the skin.
The pain was immediately preceded by a severe fever on the Thursday of the tail end of Japan’s Golden Week succession of public holidays. I had no other symptoms such as a cough or a runny nose—just a high fever that hit me like a ton of bricks and caused me to sleep for more than 15 hours straight. When I woke up on Friday the fever was gone, but I started to feel pain in my lower right leg. Like how most people would react, at first I shrugged it off and figured that it would simply go away on its own.
It did not.
The next morning the pain was worse, my leg was swollen, and in various spots the surface of the skin had turned bright red. At this point I figured that it would be wise to get it checked-out at the small, local hospital near our home. Due to the holidays, the hospital was short-staffed, but they had some out-patient clinics still operating. On Saturday afternoon I saw a general surgeon who had been assigned to the surgical out-patient clinic on that day, and he correctly diagnosed the condition as cellulitis after running a blood test. I was sent home with a prescription for oral antibiotics and a pain killer with instructions to return first thing on Monday morning when the hospital would be fully operating again. I dutifully took the medicine through Sunday afternoon, but by this time the pain had become almost unbearable and most of my right lower leg had turned bright red. This was not a good sign.
Although our neighborhood hospital was closed on Sunday, their emergency room was, of course, still open. I saw the sole physician on duty, and he counseled me to continue to take the oral medication. While his preference was to have me admitted as an in-patient, they did not have an open bed or enough nursing staff. Thus, once again I was told to go home, rest, and simply come back first thing in the morning on Monday.
I figured that I could somehow endure another night, but I was, in fact, getting more than a little concerned. At around 8 p.m. on Sunday evening the physician that had initially seen me on Saturday called me at home to ask how I was doing. He had heard from his colleague on duty in the emergency room that I had come back to the hospital several hours before and was worried about my condition.
“If the symptoms keep getting worse, your leg could turn gangrenous, and it may, ultimately, need to be amputated!” – The general surgeon whom I had met the previous day told me over the phone
Say what? There is a potential need for amputation? Just a couple of days ago everything was just fine. How could this be the case? Well, that certainly got my attention.
We subsequently discussed the merits of seeking care at a bigger hospital in the larger town about 45 minutes away, and it did not take long to conclude that this would be the safest course of action. (If there was ever such a thing as a “no-brainer” type of decision, this was it!) The promise of getting relief from the pain was a strong motivator, too.
The physician at the local hospital near our home promised to get me an official referral, which is common practice in Japan, and told me to wait for a call back. Although it seemed like an eternity, it did not take long for the director of nursing to call back. She wanted to know how long it would take for me to get to the hospital to which I had been referred. I grabbed some stuff for an overnight stay, and rushed to this major medical center. As there was almost no traffic on Sunday night, I arrived at the emergency room at about 10 pm right on time. A member of their emergency room was waiting for me by the door. That was a promising sign.
Although I did not know it at the time, I had lucked out because the physician that had been assigned to my case, who just happened to be on emergency room duty on that Sunday night, was a reconstructive plastic surgeon with a specialty in treating problems that involve the legs and feet. He ordered blood tests and immediately put me on a regimen of powerful antibiotics to be administered intravenously. The results of one of the blood tests from Sunday night, which had now become early Monday morning, were compared to the blood test results from the previous day recorded by our local hospital. They confirmed the diagnosis of cellulitis.
I vaguely recall being asked whether I wanted a private room to which I said, “Yes,” but being told that none were currently available. Thus, at some point around 2 am on Monday morning I was transferred to a 4-bed room in the ward for plastic surgery. My bed, which was partitioned off from my neighbors by thin curtains, became my whole world until Wednesday afternoon.
The doctor had left orders that I was to remain in bed and not put any weight on my right leg. My leg was, in fact, supposed to be kept elevated and continually packed with ice. As there was still a lot of swelling, pain, and redness, I was ready to comply with those orders without making any fuss at all!
Unintended consequences: One of the practical implications of those “doctor’s orders” was, however, that I was not able to get up on my own to walk to the toilet, which was located right outside my mini-Nightingale ward. Thus, every time I had the need to go, first I had to call for a nurse to help me stand up and transfer to a wheelchair simply to be rolled only about 5 meters (approximately 15 feet) to the toilet. Once there I would then have to repeat the whole procedure in reverse. This was complicated by the fact that I was hooked up to a continuous intravenous (IV) drip for nutrition and fluid replacement. In any case, after doing “my business,” I would press the call button for a nurse to help me go through this whole routine yet again simply to get back to bed. Unless you have had a similar experience, which to this point I had not, you may not appreciate the amount of effort it requires just to complete this relatively simple procedure. By the time I would get back from each mini round-trip to the toilet right next door, I was exhausted.
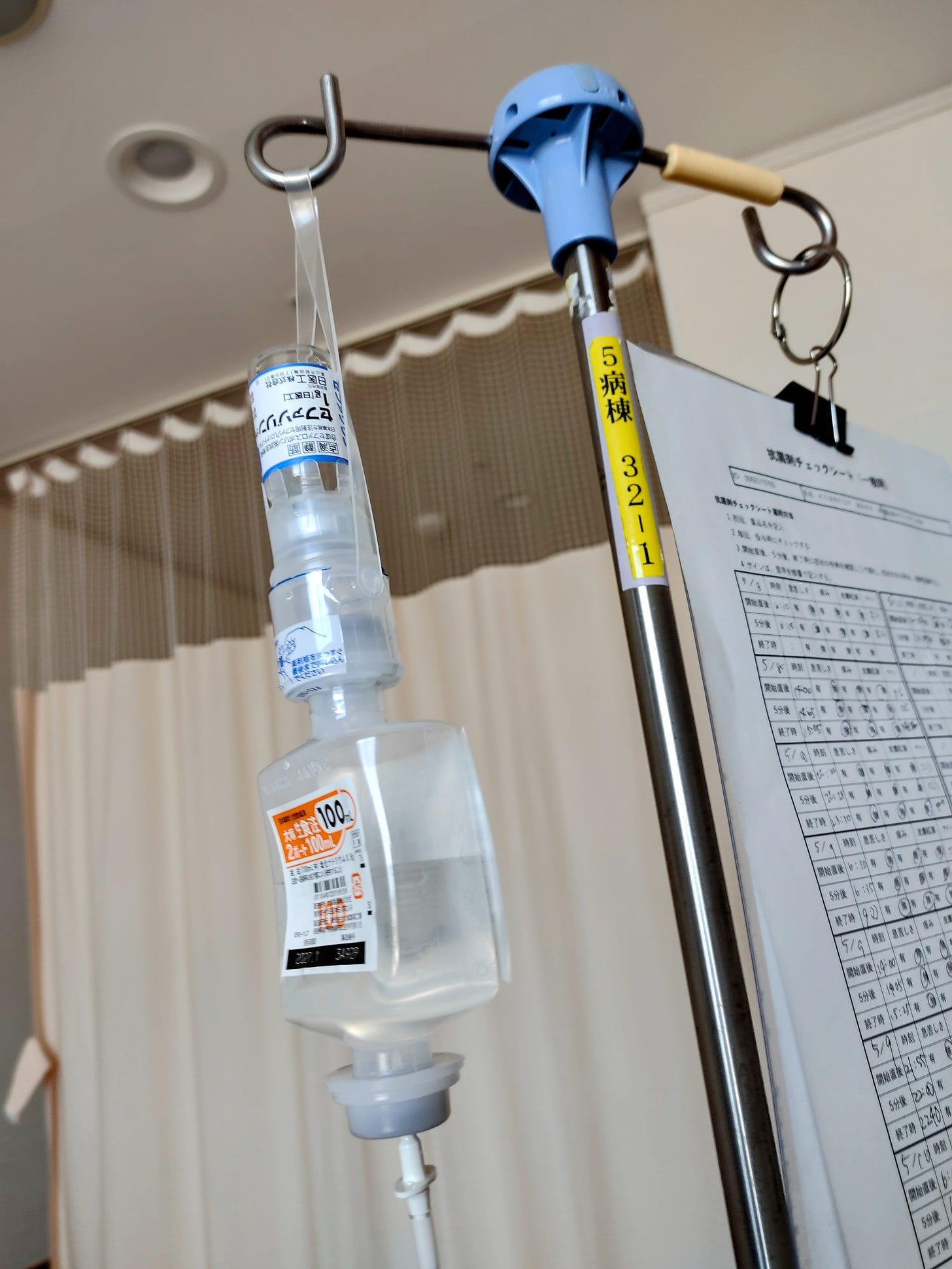
The powerful antibiotic cefazolin sodium, which is, apparently, the traditional “first line of defense” for cellulitis, was added to the IV drip 3 times per day—first at 6 am, next at 2 pm, and one more time at 10 pm. It would take about 1 hour to inject this medicine into my system one drop at a time. My physician ordered this treatment to continue for the next full week.

I was able to eat regular hospital food for breakfast, lunch, and dinner. While the quality of Japanese hospital food varies, no doubt, by facility, the hospital where I was an in-patient had reasonably good food. I was given a “standard” meal, which included 200 grams (7 ounces) of rice with a small main dish and a few side dishes for each meal. You “get what you get,” as there were no choices. Most meals were composed of some combination of fish, tofu, salad, miso soup, and steamed vegetables. A few meals included grilled chicken, and one lunch was curry rice. That was a popular one on the ward! A side benefit to my new, restricted diet was that I ended up losing 5 kg (11 pounds) over the course of 6 days.

Although I could have all of the green tea that I could drink, each meal was also served with a 65 gram (2.3 ounce) mini bottle of a “lactic fermenting beverage” called Fresh Luna, which is a perennial favorite in Japan. (Each time I took a swig of it—which does not take long to finish off considering the ultra-small package—the fact that I was consciously imbibing another type of bacteria into my body did, in fact, cross my mind. I figured that it was a good kind of bacteria, however. So far, so good!)
For the next couple of days life was very much the same. I got used to the routine, while my leg slowly started to recover.
As my physician forbade my use of the communal shower—for fear that I might cause further damage to my leg—I was limited to the equivalent of a sponge bath. The Japanese have a wonderful solution to this problem. It is an extra-long hot towel or oshibori (おしぼり). These are disposable non-woven towels that are steamed inside a plastic wrapper. One was delivered first thing in the morning, and two or three more were distributed later in the day. While smaller oshibori are common at Japanese restaurants, the kind used in the hospital where I stayed are 600 x 255 mm (24 x 10 inches). That is long enough to use to bathe one’s back by stretching it over your shoulder. While it is somewhat challenging to do this while confined to a hospital bed, I felt really refreshed after using these steaming-hot towels.
Turning point: On Wednesday morning (3 days after being admitted) life changed for the better. First thing in the morning they took more blood for another test. It did not take long for my physician to come back with the results. He now had 3 sets of data—including the original bloodwork done at our neighborhood hospital back on Saturday. The results indicated that 4 key components of the blood were, in particular, showing dramatic improvement. My doctor was especially pleased to confirm that there were no signs of blood clots or thrombosis, which could have led to a whole new set of problems. He described my situation as almost a “textbook case” of cellulitis. His recommendation was, however, to remain at the hospital until the weekend to continue the thrice-daily regimen of antibiotic IV therapy. Well now, that certainly sounded encouraging!
He had more good news.
First, a private room had just opened up. “It will cost a little bit extra, but would I like to transfer?” the doctor asked. It was time for another quick decision about which I had no hesitancy. “Absolutely!” I responded. Yes, there was a 5,500 yen (approximately US $41) per day premium to stay in a private room, but it was definitely worth it—if only to get more rest.

My room literally came with a view…of the sea, which was an added benefit. It also had a “unit bath” type of combination shower/toilet.
The doctor just kept the surprises coming…
I could take a shower! Yeah! I must admit that the first shower in several days felt wonderful and really helped to boost my spirits.
The rest of my stay was somewhat monotonous, which was just fine. I made a series of incremental improvements until the doctor judged me fit to be discharged on Saturday after spending a full week in the hospital.
After taking it easy for a while at home and another couple of follow-up visits to his out-patient clinic during the following week, he told me that my health should be fully restored.
While my body is now on track to return to normal, I will never forget this experience, which came as somewhat of a shock to my former sophomoric (now middle-aged) self with its sense of invulnerability.
Lessons learned: While this 10 day “adventure” is certainly a trip that I wish I had never taken, in retrospect the experience provided several valuable lessons.
Be Vigilant if You Suspect Cellulitis: While there is not a lot one can do to prevent cellulitis—especially when one’s immune system is under attack--other than patching up all scrapes and bruises as soon as possible and keeping your skin clean and moisturized, it is important to know the symptoms and take immediate action if you think something similar may be happening to you.
Where Would We All Be without Modern Antibiotics? Just recalling that fateful telephone conversation about the potential for my leg to turn gangrenous and eventually need to be amputated certainly “struck a nerve.” Where would we all be without the kind of powerful antibiotics that were used to beat back my case of cellulitis? What must life have been like before the accidental discovery of penicillin, the first modern-day antibiotic, in 1928 by Scottish biologist Alexander Fleming while studying the staphylococcus bacteria? Without a doubt life must have been much shorter and probably a lot more painful for many. An onset of cellulitis, while not necessarily a death sentence, must have meant almost certain amputation. I for one am grateful for Fleming’s work and for all of the subsequent development of modern-day antibiotics.
Head Straight to a Larger, Regional Medical Center in Case of Anything Serious: In retrospect at first I should have, of course, sought counsel at a larger, regional medical center rather than visit our local, small-scale hospital. At first I was, however, unaware of what I had and unclear just how serious this illness could be. In any case, at the risk of stating the obvious, if I suspect that I may have a serious health issue, on a go-forward basis I will skip the local hospital and go directly to the same regional medical center where I received excellent care as an in-patient.
New-found Respect for Physicians and Nurses: Looking back at this “series of unfortunate events,” I realize just how lucky I was to have met a few key people who were genuinely concerned about my health and had the knowledge and resources at their disposal to do something about it. I found a hospital by accident where there is a true commitment to providing superior customer experience, which was evident by their speedy response time, politeness and obvious pride in their work. If I ever have another health issue, I will definitely return to the same hospital. Besides the physicians, I was very well treated by every member of the nursing team and the various staff members—including the woman who brewed hot green tea for me twice a day. I won her over by responding to her question about my opinion of baseball player Yohei “Showtime” Ohtani by telling her, “He cannot be human; He must be a god.” Ohtani’s impressive career in the major league is the source of much national pride in Japan.
New-found Respect for People with Limited Mobility: Despite having a father who spent about half his life “confined” to a wheelchair without the use of his legs and working in the medical industry for almost 3 decades where I had many opportunities to interact with wheelchair-bound patients who were also customers, this was my first personal experience relying upon a wheelchair—at least for the first 3 days at the hospital. There is simply no substitute for this sort of “hands-on” experience. I now have both a new-found respect and greater empathy for physically disabled people.
Appreciation for the Japanese Ability to Live in Close Quarters While Maintaining a Degree of Personal Privacy: Despite our extremely close quarters occupying the same 4-bed room, my 3 other roommates did their best to remain quiet and respect each other’s privacy.
While for the most part my experience as an in-patient was positive, there was one incident which took place at 3:47 am on the Tuesday of my week-long stay that sticks in my memory. I remember waking up in the dead of night thinking, “What the f___ is going on?” Somebody across the hall in another 4-bed room was blasting their television. Now I am not normally one to complain, but in this case, I became “that guy” and pressed the nurse call button. I was somewhat surprised to be asked, “How can we help you?” Wasn’t it obvious? After explaining that I wanted some peace and quiet, I listened to the nurse walk across the hall to speak with the unseen perpetrator. From the sound of his voice I could tell that he was an old man, who was probably hard of hearing and, possibly, not aware of how to listen via the earphones for the television. The volume of the TV was turned down, but it did not go away completely. The nurse came back and asked, “How is that?” I explained, naturally, that it was an improvement, but I expect not to have to listen to such noise at all in the middle of the night. I have no problem with the regular sounds of a hospital such as various alarms, crash carts being rolled through the hallway, an occasional cough, etc., but I was not willing to put up with having to listen to somebody else’s television in the middle of the night. Suffice to say that we reached an understanding, and the television was turned off. I subsequently went back to bed.

Hospital Beds with a Remote Control Are Awesome! Although I simply lay flat in bed for the first night—or at least for the few hours left that evening before my first scheduled injection of antibiotics at 6 am the next morning—it did not take long to figure out how easy it is to manipulate the bed to find just the right position while keeping my right leg elevated.
Thankful for Support from Friends and Family: Based upon the above report, you may have gotten the false impression that I experienced all of this entirely on my own. That was definitely not the case, as I had support from family and friends both near and from the other side of the world throughout the recovery process. I cannot even imagine going through this sort of incident on one’s own.
What’s next: After receiving the last antibiotic IV drip injection late on Friday night, I was discharged from the hospital on Saturday morning. The doctor expects me at his out-patient clinical in about 6 days from now for a check-up. Wish me luck, although I seem to be on track for a speedy recovery. I am, however, not going to push it and simply take it easy for a while.
Thinking “big picture,” we should all be fearful of the likely development of antibiotic-resistant bacteria. The type of antibiotic that literally saved my skin this week was cefazolin sodium, a first-generation cephalosporin, which means it is one of the earliest types of drugs in the class of cephalosporins that date back to the 1950s. While there are, apparently, alternatives, I would hate to think of a day when we run out of alternative antibiotic treatments.
While I never want to go through something like this again and intend to stay out of the hospital for as long as possible, especially as I get older, it is inevitable that I will find myself back to being an in-patient for something at some point in the future. Thus, I am going to treat this week’s incident as basic training for a—hopefully--distant tomorrow.
Final note: While this experience certainly shook me to the core, I am recovering. My ordeal pails in comparison to the struggles of some of the other patients at the hospital with whom I was exposed and all of the countless other people who are grappling with more series illnesses. Thus, I count myself lucky!
#cellulitis #antibiotics #ivdrip #hospitalstay #inpatient #bacterialinfection #蜂窩織炎 #抗生物質 #点滴 #入院患者 #細菌感染症










Your other article of shortage of factors brought me to this article and I really had no idea you had gone through that. Having dealt with cellulitis three times myself I can appreciate all your takeaways and I think you’ll appreciate this short story. One of the times I had cellulitis was around my stoma and spreading larger around my abdomen, I went to the hospital immediately and the nurse recognized me as having given a talk the night before at a special nurse meeting. (Luckily, she loved it. Ha ha) She told the hospitalist right away that they had to figure out a solution for me because I had to get to Iowa in four days to give my next funny talk for healthcare professionals. Within 2 days the discovered the right antibiotic and I was out of there. My husband had set up a bed in our van, and we took the 6 Hour drive to my next presentation with pills in hand. I loved everything about this article from the food descriptions, your painful process, your room situation and mostly your appreciation for the healthcare professionals. Thank you for sharing.
I often have to control or guide doctors what to do here, as there is no GP institution as such. Often ended up passing like a ball to different specialists until researched myself and asked “ give me referral there” , then solved. For big issues still go to Australia if not urgent . But care in Japan is good, important to get to the right specialist and clinic which is on you , mostly ( my experience only).